Contents
- 1 Brushing
- 2 Flossing
- 3 Choosing a Brush
- 4 Choosing a Toothpaste
- 5 Mouthwashes
- 6 Bad Breath
- 7 Whitening
- 8 Cavities
- 9 Dental X-rays
- 10 Periodontal Disease
- 11 Pregnancy and Dental Care
- 12 Dental Care for Your Infant or Toddler
- 13 Tooth Eruption
- 14 Nursing Bottle Syndrome
- 15 Hazards of Thumbsucking
- 16 My Child is Getting a Second Row of Teeth!?!
- 17 Sealants
- 18 What to Do if a Tooth Gets Knocked Out
- 19 Wisdom Teeth
- 20 Loose Dentures
- 21 Diabetes and Oral Health
- 22 What To Do After a Tooth is Extracted
- 23 Acid Erosion
- 24 Your Dental Insurance
- 25 Dental Implants
- 26 Infection Control
- 27 Fluoride in Tap Water
- 28 TMJ Disorders
- 29 The Power of a Smile
Brushing

Brushing is one of the effective ways of removing harmful plaque from your teeth and gums. Dental plaque is a film of food debris, bacteria and bacterial products that forms on your teeth. Once plaque is removed, it begins the process of forming again and therefore needs to be removed on a continuous basis. Dental plaque is an essential component to causing cavities and periodontal / gum disease. No plaque means no cavities or gum disease. Unfortunately, the moment it is removed it begins the process of reforming. Also, since it coats all parts of the teeth and gums, it also forms in hard to clean areas.
Since the dental plaque is continually forming, there is no current cure for cavities or periodontal / gum disease. Prevention is largely a matter of keeping the plaque levels under control.
Getting the plaque and food debris off your teeth and gums in a timely manner prevents the bacteria in the plaque from converting parts of the food you eat, into cavity causing acids.
Brushing two to three times a day is required to keep the plaque levels under control.
Brushing techniques
Everyone’s teeth are different and present their own issues or complications. There are a variety of brushing techniques and types of brushes that can be used. Your dentist or hygienist can make recommendations specific to you.
Some popular techniques that work are:
- Use a circular motion to brush only two or three teeth at a time, gradually covering the entire mouth.
- Place your toothbrush next to your teeth at a 45-degree angle so that the bristles of the brush can also clean inside the pockets or space between the tooth and the gums. Gently brush in a circular motion, not up and down. This circular motion causes less wear on your tooth structure and gums. You should brush all surfaces of your teeth – front, back, top, and between other teeth, rocking the brush back and forth gently to remove any plaque growing under the gum.
- Don’t forget the other surfaces of your mouth that are covered in bacteria – including the gums, the roof and floor of your mouth, and most importantly, your tongue. Brushing your tongue not only removes trapped bacteria and other disease-causing germs, but it also freshens your breath. Instead of a brush, a tongue scraper can also be used on the tongue.
- Remember to replace your brush when the bristles begin to spread because a worn toothbrush will not properly clean your teeth.
- Effective brushing usually takes about two to three minutes.
Keep in mind that while essential, brushing only does part of the job of cleaning teeth and gums. In order to adequately clean all areas, floss must also be used. Otherwise all the plaque and food debris that you are cleaning off with the brush, continues to sit undisturbed in areas between the teeth that brushes don’t reach.
__________________________________________________
Flossing

Floss is a string or cord like material that is used to clean in between the teeth where the toothbrush cannot reach. Just as with the toothbrush you are mechanically scraping the plaque off the teeth on a regular basis to prevent the problems with cavities and periodontal / gum disease, that dental plaque cause.
Many of us were brought up with mom’s constantly asking if we brushed out teeth and so often don’t think twice about making sure to brush. Unfortunately, the checking to see if we flossed our teeth was not as frequent or may not even have occurred. For this reason, flossing for many people is not an ingrained habit like brushing. Flossing is as important, if not more important than brushing when it comes to cleaning your teeth. This is a message that is reaching the general population more frequently now and is gradually leading to improved prevention of dental diseases.
To use the floss, you would break off a piece of floss about 18 inches long. You wind the majority of the floss around the middle finger and the remaining floss around the same finger on the opposite hand. It is this finger that would take up the floss as it gets used. You then use your two forefingers or a forefinger and thumb to guide the floss. If the floss begins to fray in an area, unravel some off one finger and take up the slack on the finger on the opposite hand so that you have a new portion of the floss between your fingers to work with.
Once you place the floss between the teeth, you would wrap it around the tooth making a “C” shape. Then push the floss up and down making sure it goes below the gum line. There is a space between the tooth and the gum before the gum actually attaches. This space is often referred to as a pocket or sulcus. The floss is slid into the pocket or sulcus for the teeth on both sides of the space. Care is taken to make sure that the floss conforms to the shape of the tooth so that it slides freely in and out of the space. You have more control and this is easier to do with your fingers right up to the tooth using a shorter area of floss.. Demonstrations and photos such as the one above don’t make this clear as the fingers controlling the floss are usually shown farther apart so that you can see where the floss goes. It is meant as a demonstration of where floss is used but If you actually floss as it shows in the picture you get a lot of movement of the floss out by your fingers but not much on the tooth itself. You have much better control and are far more effective with the fingers controlling the floss being right up by the tooth.
To floss in between teeth with braces or bridges in place you have to thread the floss under the wire or artificial tooth to get it in place. A device called a floss threader can be used to do this. This is basically a plastic loop with a stiffer straight portion. The floss is inserted through the loop of the floss threader and then the threader is “threaded” or pushed under the orthodontic wire or artificial tooth on the bridge and used to pull the floss with it. Once the floss is through the space you then remove the floss threader from it and floss normally.
It is recommended to floss daily. Flossing should be done prior to brushing and should normally take no longer than 3 mins. to complete. Like any skill, the more you do it the faster and more efficient you get at the task.
There are a variety of types of floss on the market. There is also waxed and unwaxed floss. The waxed floss tends to shred less easily and is often used when the contacts between the teeth are tighter. Studies have shown that waxed or unwaxed floss work equally well and for many people it is just a choice based on personal preference. Some floss is woven, some comes in pre-sized sections with the floss wider or fatter at one end than the other. Some floss is attached to small holders or picks for use by people that find it difficult to hold with their fingers.
_________________________________________________
Choosing a Brush

When you get down to the basics, a toothbrush is really just a way to scrape a sticky thin film (dental plaque) off of the tooth. It is bristles on a stick or handle of some sort. With all of the high tech, new and improved brushes highlighted in commercials and advertising it is sometimes useful to keep this in mind. Having said that, there are certain things you want to look for.
You want a head (the part with the bristles) on the brush that is not too large so that you can get it into all areas of the mouth easily. You want a brush that is soft or extrasoft. These are still stiff enough to remove plaque but do less damage to the teeth and gums over time.
Along with brushes available for the standard job of brushing your teeth there are also brushes designed for specific problems or situations. For example there are brushes called proxabrushes that are designed to fit into larger spaces between teeth. These spaces are either from the loss of a tooth and having the other teeth shift to only partially close the space, or from the recession of the bone and gums from periodontal / gum disease.
Some brushes have bends in the handles to help you to try and reach the backs of teeth at the back of the mouth.
There are brushes designed for cleaning dentures as well.
Another popular choice is the electric toothbrushes. If we again look at our initial statement about the basics of what you are trying to do, you realize that an electric brush does not do anything that you cannot do with a less expensive manual brush. They can still be a nice option though. Consider the difference between scrubbing a floor with a manual brush or using an electric floor cleaner. Some people also just find them easier to use for a variety of reasons. These reasons include, but are not limited to, problems with manual dexterity due to things like tremors or strokes.
Some people even use an electric brush at home as a matter of preference and use a manual toothbrush when they travel for ease of packing.
______________________________________________________
Choosing a Toothpaste

There are a wide variety of toothpastes on the market. Choosing the one for you can seem like a daunting task. It may be helpful to consider what toothpaste does from the most basic and move up from there to select the properties you want for your specific situation.
If we go back to our basic purpose of brushing, which is physically scraping a thin sticky film of bacteria and food debris off of the teeth, you realize you can do this without toothpaste at all. It would however, be like scrubbing a sink with just a brush rather than with a brush and an abrasive cleaner. You can do it, but it is faster and more efficient to use the cleaner with the brush.
At their most basic, toothpaste contains an abrasive, a binding agent to hold the abrasive together, and a flavouring agent. What varies after that is the additives. You can go even more basic than this and many people do, by using baking soda alone to brush with. This is essentially using an abrasive, without the binding agent and the flavouring agent.
The most common additive to the basic toothpaste is fluoride which is added to decrease the incidence of cavities. The fluoride works by reacting chemically with the hydroxyapatite in the enamel and dentin. Hydroxyapatite is the main structural mineral form in enamel and dentin. The fluoride changes the hydroxyapatite into fluoroxyapatite which is less soluble in acid. This means the mineral in the tooth is then more resistant to the acid produced by cavity causing bacteria that dissolves the mineral away to form cavities.
Fluoride then, can be a good additive to have in the toothpaste you choose to help prevent problems from cavities and from damage from acidy foods, both of which dissolve the mineral out of the tooth. Fluoridated toothpaste is not recommended for very young children. The levels of fluoride in toothpaste are designed for use as a topical application and are deemed to be healthy and safe for this normal use. With very young children however, they often end up eating a fair bit of toothpaste and so are ingesting more fluoride internally than you would get topically on the tooth. This can lead to too much fluoride. It may cause small whitish permanent areas of discoloration on the teeth from the excess systemic fluoride while the teeth are forming. Ingesting even higher levels of fluoride can cause other problems with teeth and other things but are not noticed from just swallowing some excess toothpaste. Once children are old enough that they are not eating a lot of the paste, toothpastes with fluoride are fine and recommended for most people.
Some toothpastes also add chemicals to reduce the formation of tartar or calculus.
Chemicals in the form of some form of a peroxide are also often added as a bleaching or whitening agent. It used to be that toothpastes that claimed greater whitening power, had a greater abrasiveness which also causes more wear on the teeth. Currently, most toothpastes that claim whitening properties are usually doing it through the addition of bleaching chemicals.
Other pastes have additives to reduce sensitivity or to promote adding mineral back into the tooth (this is again on a microscopic level and won’t reverse anything large enough to notice visually but can help offset early mineral loss from acidic foods and drinks).
The more chemical agents that are added to a toothpaste usually means a higher price for the paste.
The other large factor in price on toothpastes is advertising. In general, toothpaste manufacturers that advertise more have a higher cost structure and higher price on the toothpaste.
The more additives you have in the toothpaste, the more it begins to resemble a chemical soup with greater and greater chances of having an adverse reaction to something in the paste. If you notice your gums get more sensitive with a particular toothpaste or some other problems develop, try switching to a simpler paste with fewer additives and see if that makes the problem disappear.
As a final note about toothpaste, photos and advertising images of a toothbrush with lots of toothpaste look visually appealing and imply that that is how much you should be using but this is not so. You only need about a pea sized amount of toothpaste on your brush to do a good job. Manufacturers show more because it is easier to see and it sells more paste.
_________________________________________________________
Mouthwashes

There are a wide variety of mouthwashes on the market. For the most part they are useful as an agent of freshening the breath by masking it with other strong fresher smelling odors.
Bad breath can have a variety of causes, such as certain foods, high levels of bacteria, active gum disease, or certain medical problems or disease states. If the bad breath is caused by active gum disease, reducing the levels of bacterial plaque can help with mouth odor and it is also helpful in reducing gum disease and cavities.
Manufactures have also followed the path of toothpastes in that they have come up with a wide variety of formulas with the same chemical additives that you can get in different toothpastes.
Most claims of reducing bacteria by mouthwashes are not supported in research studies not performed by the manufacturers. As a typical example, one leading mouthwash manufacturer proudly claims that their product reduces the amount of bacterial plaque on teeth by 50% over not rinsing with their product and in this case even quoted an independent study that was not funded by them. What they failed to mention in their claims is that in the study, there were three groups, not two. One group did not rinse with anything, one rinsed with the manufacturer’s mouthwash and a third group rinsed with water. Yes in the study, rinsing with this particular brand of mouthwash did reduce the amount of bacterial plaque by 50% over not rinsing at all, but rinsing with water reduced the levels of bacterial plaque by 51%. The reduction in plaque levels noted was due to the actual act of rinsing with any liquid. The mouthwash manufacturer neglected to mention that part of the study.
One mouthwash that is more effective than just the rinsing action at reducing the amount of bacterial plaque is Chlorhexidine mouthwash. It is available in Canada only by prescription due to the levels of antibiotic in it. Chlorhexidine has long been the best mouthwash available to reduce bacterial plaque levels in patients but it has side effects. Patients often dislike the staining of the teeth that occurs but this can be removed at regular dental cleanings. Other side effects like diarrhea and vomiting sometimes occur. As well, there is the whole problem of developing antibiotic resistant strains of bacteria.
Another inexpensive and natural option is available. Recent studies have shown that using green tea as a mouthwash will actually reduce bacterial plaque levels better than prescription level Chlorhexidine mouthwash and it also aids in the reduction of bad breath. All this is done inexpensively and without the side effects of an antibiotic. Staining of the teeth can still be a concern with tea but this can also be managed by your dentist and hygienist with regular care.
__________________________________________________________
Bad Breath

Bad breath (halitosis) can be an unpleasant and embarrassing condition. Often we don’t even realize we have it unless someone else tells us. It is something however that everyone has from time to time, especially in the morning.
There are a variety of reasons you may have bad breath, but in healthy people, the most common reason is due to bacteria on the tongue, especially the back of the tongue. Some studies have shown that simply brushing the tongue or using a tongue scraper can reduce bad breath by as much as 70 percent.
Some possible causes of bad breath?
- Morning time – Saliva flow almost stops during sleep and its reduced cleansing action allows bacteria to grow, causing bad breath.
- Certain foods – Garlic, onions, etc. Foods containing odor-causing compounds enter the blood stream; they are transferred to the lungs, where they are exhaled.
- Poor oral hygiene habits – Food particles remaining in the mouth promote bacterial growth.
- Periodontal (gum) disease – Colonies of bacteria and food debris residing under inflamed gums.
- Dental cavities and improperly fitted dental appliances – May also contribute to bad breath.
- Dry mouth (Xerostomia) – May be caused by certain medications, salivary gland problems, or continuous mouth breathing.
- Weight Loss – dieting, particularly low carb diets can lead to ketosis which can cause bad breath.
- Tobacco products – Dry the mouth, causing bad breath.
- Dieting – Certain chemicals called ketones are released in the breath as the body burns fat.
- Dehydration, hunger, and missed meals – Drinking water and chewing food increases saliva flow and washes bacteria away.
- Certain medical conditions and illnesses – Diabetes, liver and kidney problems, chronic sinus infections, bronchitis, and pneumonia are several conditions that may contribute to bad breath.
What can I do to prevent bad breath?
- Practice good oral hygiene – Brush at least twice a day and floss daily to remove food debris and plaque from in between the teeth and under the gumline. Brush or use a tongue scraper (a small tool found in most drug stores in the dental section) to clean the tongue and reach the back areas. Replace your toothbrush every 2 to 3 months. If you wear dentures or removable bridges, clean them thoroughly and place them back in your mouth in the morning.
- See your dentist regularly – Get a check-up and cleaning at least twice a year. If you have or have had periodontal disease, your dentist will recommend more frequent visits.
- Drink water frequently – Water will help keep your mouth moist and wash away bacteria.
- Use mouthwash/rinses or breath mints –These tend to only give symptomatic relief for a short time by masking the odor with a different more pleasant odor. If you are using breath mints be sure to use ones that are sugar free. Mints with sugar can cause severe cavities, especially with people with dry mouths.
In most cases, your dentist can treat the cause of bad breath. If it is determined that your mouth is healthy, but bad breath is persistent, your dentist may refer you to your physician to determine the cause of the odor and an appropriate treatment plan.
_________________________________________________
Whitening

Whitening, or as it is sometimes called, bleaching, for teeth is a process to reduce stain in a tooth and lighten the colour. Surface stains can usually be removed with a dental cleaning and polish. Some stains however are deeper in nature. The enamel is about 98% mineral and the mineral does not change colour. The 2% organic portion though can absorb stains over a period of time and cause the teeth to darken.
To whiten the teeth, a bleaching process is used. Bleaching in this context refers to the chemical nature of the reaction that goes on and does not refer to using household bleach, even diluted, to whiten the teeth. Much safer products using a carbomide peroxide (also not identical to hydrogen peroxide) are used. These products are very safe when used in the mouth.
As mentioned the whitening gels are quite safe but they can cause increased tooth sensitivity in some people. If they do cause increased sensitivity, this will go away with a bit of time once the whitening is discontinued. If they find their teeth getting sensitive, patients can either discontinue the whitening process or they can try using the whitening gel every other day instead of every day for a period, or every third day, whatever schedule gives them results without the sensitivity. It takes longer but you still get the whitening. In patients with severe sensitivity even before doing whitening it is probably not a good idea to try.
Differences in products for whitening almost always use the same types of chemicals in a gel form but differ in how they apply the gel or hold it next to the teeth.
Over the counter strips for example, still use the same chemicals as other methods but use a strip that is applied to the teeth to hold the chemicals in contact with the teeth. These can be a relatively effective and inexpensive options and are an option for patients to do on their own. The strips tend to work better in the front of the mouth and do not stay in place as well in the back areas of the mouth. If all you want to do is to lighten up your front teeth, these can be a good method to choose.
Another option is to have small flexible plastic forms customized to the shape of your teeth and to apply a whitening gel inside the trays and wear them at home. This option is more expensive than the over the counter strips but works better for whitening all of the teeth. The trays with the whitening gel can be worn overnight but many people have a tooth grinding habit without realizing it and can quickly destroy the custom trays. Wearing the trays with the whitening gel for about an hour during the day works well and has far fewer problems with tray wear. The trays are worn with the gel for about an hour a day for a week or two. Afterwards they can be used periodically every 2 – 6 months for a short period to bleach out any new staining that is occurring and to keep an optimum whitened shade to your teeth.
A third option is to have the whitening completed in the office during one or more visits using a combination of a whitening gel and a special light. This option is usually the most expensive option. The results are faster but in any studies not funded by the manufacturer of the special lights, there appears to be no improvement in whitening over using the custom trays at home.
It is possible to overbleach the teeth but it takes a LOT to do that. Following the recommended periods of usage time result in no problems other than the occasional reversible sensitivity.
While the above describes the basics of whitening or bleaching there are a few things to realize. One, teeth are not naturally pure white. They tend to have a slight yellowish or grey tone naturally. If you see someone with totally white teeth they are usually either artificial or have been artificially whitened. Images in media such as magazine photos, television and movies tend to show large numbers of models and actors with artificially white teeth. This is fine, but it does not mean your teeth are abnormal if they don’t match the colour of teeth you see on models and actors.
There are shade guides which are used to match the colour of “white” filling material to a person’s natural teeth so they blend in better. It is an easy matter to compare the colour of the patient’s teeth with the usual and normal colours that we see in teeth. This can at least let you know if your teeth are darker than “normal”. It is just a matter of patient preference as to whether you decide to whiten your teeth. It does no long term damage to the teeth as long as instructions are followed.
Some things do not bleach or whiten on a tooth. Tooth coloured fillings for example will not whiten. When they were placed they were matched to the colour of the teeth. If the teeth are lightened then any fillings of this type that you can see will look darker than the tooth. This can be changed by changing the fillings and matching them to the new colour of the teeth but this involves more cost and normally removing yet more natural tooth as the filling is replaced. If the teeth have darkened from when the fillings were placed, whitening may lighten the teeth enough to match the previous lighter colour of the fillings. The above is true for other forms of restorations as well, such as veneers, crowns, bridges, and partial dentures.
As a general rule, yellowish or brownish discolouration will whiten better than grayish tones on teeth.
Also, some conditions such as tetracycline staining from a particular antibiotic used while the teeth were forming may have improvement but not whiten totally.
__________________________________________________
Cavities

First, what is a cavity? Bacteria in the dental plaque which forms on the surface of teeth feeds on sugars in your diet and produce an acid waste product. This acid waste product dissolves the mineral out of the tooth in the area where the bacteria are sitting on the tooth. Tooth enamel is 98% mineral and the dentin under the enamel is about 70% mineral. The loss of mineral causes a hole in the enamel and a soft mushy sided hole in the dentin. The bacteria continues to grow in the hole and cause it to deepen.
There are three things that are required for cavities to form. These are; dental plaque, sugar and a tooth. It takes all three. Remove or reduce any one and you reduce the overall incidence of decay.
Dental Plaque
We have already talked a little bit about dental plaque in the sections on brushing and flossing. Dental plaque is formed by a combination of bacteria and food debris on the surface of the teeth. The plaque forms on all areas of the teeth, even between the teeth and on the roots to the bottom of sulcus of the gums around the teeth. If you remove all of the plaque, new bacteria settle on the teeth and begin to grow and form a new layer of plaque right away. The whole purpose of brushing and flossing is to mechanically scrape the plaque off of the teeth so it is not present to cause cavities (and periodontal/ gum disease but more on that in another section).
Since it is bacterial in nature, a variety of methods of using antibiotics in some form have been tried. With oral rinses or mouthwashes with antibiotics you can reduce the levels of dental plaque but the antibiotics do not limit themselves to only the bacteria in dental plaque but also reduce other helpful bacteria. You also get antibiotic resistant bacteria developing. If you could treat the bacteria once with the antibiotic and have the problem solved, fine, but as we have mentioned the dental plaque reforms every day.
Some attempts using an antibiotic in a plastic varnish which is painted on the teeth have had some success in the past. Doing this they are trying to use a lower dose of antibiotic and to contain it to the surface of the teeth to try and target the specific bacteria in dental plaque. It is a form of treatment that never really caught on well and the varnish would wear over time causing patients to complain about the rough or chipping varnish remnants being uncomfortable to the tongue. I am not sure if the company promoting this treatment is still in business or not.
The specific bacteria that contributes most to cavities is Streptococcus Mutans. There has been research into ways to try and specifically target this bacterial species. I have read articles in dental journals saying that a vaccine against Strep. Mutans would likely be developed within the next two years or so. Unfortunately these were written thirty years ago so this solution does not seem as promising as they expected and was not as easy as originally thought.
One thing of note, even though you are dealing with the bacteria causing cavities, they are still contagious. Different people will have higher or lower levels of the cavity causing bacteria in their mouths as shown by taking saliva samples and culturing them. These levels are not solely dependent on brushing and flossing. There is differences in the actual amount of the bacteria in the saliva. More bacteria in the saliva means more settles on the teeth to form dental plaque. It is not uncommon for a child with a low incidence of cavities to have low levels of cavity causing bacteria in their mouths to begin with. This can change over time through cross contamination from other people.
Sugar
The reason sugar is required for cavities to form is that is what the cavity causing bacteria are eating and metabolizing into acid. Reducing or eliminating sugar, reduces or eliminates cavities. The only living creatures on the planet to develop cavities are humans, animals kept as pets and fed human food with sugar, and bears that eat a lot of honey.
As human society developed and sugar in various forms became more common in diets, the incidence of cavities has increased.
Sugars in stickier foods are worse as they hold the sugar in place on the tooth longer. Things like braces, partial dentures or large fillings can make it easier for sugars to get trapped on the tooth in hard to clean areas.
When speaking to patients with a high incidence of cavities and recommending a reduction in sugar intake they often say “I eat very little sugar and don’t eat a lot of candy”.
Sugars are a type of carbohydrate sometimes called “simple carbohydrates”. Sugars occur naturally in many foods, especially fruits, but manufacturers also add sugars to most processed foods these days, because people seem to buy more sweet foods.
Sugar is present in foods in many forms and under many names. You are often getting far more sugar than you realize in processed foods. Food labels are supposed to list the ingredients in order of percentage of the total ingredients but it is common for food manufacturers to try and make a product look like it has less total sugar by listing sugars under a variety of different names.
Careful reading of labels is necessary to know how much added sugar you are getting. Sometimes there will be small amounts of many types of sugars, so none of them end up being in the first few ingredients of the label. Other times, sugar masquerades as apparently more “healthy” ingredients, such as honey, rice syrup, or even “organic dehydrated cane juice”. These are sugar. Sometimes fruit juice concentrates will be used, which sound wholesome, but usually the juices chosen, such as white grape, apple, and pear juices, are among the least nutritious of the juices. By the time they are “concentrated”, very little remains but the sugar. Here is a list of some of the possible code words for “sugar” which may appear on a label. Hint: the words “syrup”, “sweetener”, and anything ending in “ose” can usually be assumed to be “sugar”. If the label says “no added sugars”, it should not contain any of the following, although the food could contain naturally-occurring sugars (such as lactose in milk).
- Agave Nectar
- Barley Malt Syrup
- Beet Sugar
- Brown Rice Syrup
- Brown Sugar
- Cane Crystals (or, even better, “cane juice crystals”)
- Cane Sugar
- Coconut Sugar, or Coconut Palm Sugar
- Corn sweetener
- Corn syrup, or corn syrup solids
- Dehydrated Cane Juice
- Dextrin
- Dextrose
- Evaporated Cane Juice
- Fructose
- Fruit juice concentrate
- Glucose
- High-fructose corn syrup
- Honey
- Invert sugar
- Lactose
- Maltodextrin
- Malt syrup
- Maltose
- Maple syrup
- Molasses
- Palm Sugar
- Raw sugar
- Rice Syrup
- Saccharose
- Sorghum or sorghum syrup
- Sucrose
- Syrup
- Treacle
- Turbinado Sugar
- Xylose
When you include all of the hidden sugars the average person in North America consumes 15 teaspoons of sugar a day.
Sugar can contribute to a wide range of other problems as well, including obesity and diabetes but we are focusing just on the cavities here for now.
Remember, your body and the cavity causing bacteria don’t care what the label says, it’s all just “sugar”.
Teeth
As mentioned, teeth are also required for cavities to form. This means cavities will not form on dentures, implants or fillings. With large fillings though, any tooth that is left is still prone to cavity formation. Often patients will say that they can’t possibly get more cavities because there is almost no tooth left, it is almost all fillings. While they may have a lot of fillings, if there is any tooth left at all, it can get a cavity.
___________________________________________________________
Dental X-rays

Dental radiographs are commonly called x-rays. Many diseases of the teeth and surrounding tissues cannot be seen visually without them. Dental x-rays can help diagnose problems early when they can be treated more easily and prevent larger problems. For example, many cavities can be seen easily in the mouth but others can develop in areas that the dentist can’t see and can get large enough that the first sign of them is the tooth abscessing and needing either extraction or a root canal treatment. Lesions inside the bone can also not be seen without x-rays. Radiographs show the condition of your teeth, their roots, jaw placement, and the composition of your facial bones. They can help detect the presence or degree of gum disease, abscesses, and abnormal growths.
There are different types of dental x-rays. Some are smaller and used inside the mouth and some are larger and have the film positioned outside the mouth. Most people are more familiar with the smaller ones used inside the mouth to help diagnose cavities.
When x-rays should be taken and how often will vary between patients and the type of x-ray. They may be recommended as often as every six months or more commonly every two years or longer for adults.
The Ontario Dental Association as well as the Canadian and American Dental Associations all agree that how often dental x-rays should be taken depends on a number of factors such as your present oral health, your age, your risk for disease and any signs and symptoms of oral disease you may be experiencing. For example, children may require x-rays more frequently than adults. This is because their teeth and jaws are still developing. Also, their teeth are more likely to be affected by cavities than those of adults and since their teeth are smaller, problems become more serious much quicker.
Most conventional dental x-ray machines use high-speed film, which reduces your exposure to radiation, plus some dentists, including ourselves use digital x-rays which use about 80 percent less radiation than conventional ones. In general, dental x-rays emit lower levels of radiation than other medical x-rays. Mammograms, for example, send out five times more radiation than dental x-rays and a chest x-ray can use over 200 times the radiation of dental x-rays.
Having said all that, radiation in too high a level can be harmful. You must balance the risks with the benefits at all times. For this reason all attempts are made to reduce the amount of radiation as a general safety measure. X-ray machines are inspected regularly to ensure they are working properly. Lead aprons are used to minimize radiation to any areas where they are not required. For dental x-rays the risks are almost always outweighed by the benefits.
To help minimize any radiation not required please advise your dentist if you have had any recent x-rays in another office as a copy can be requested and if the existing ones provide the information needed, and are recent enough, then new x-rays may not be needed. Your dentist should also know of any other x-rays or radiation you have had for medical treatment or tests.
If you are pregnant or suspect you may be pregnant make sure you notify your dentist. Fetuses during development are more susceptible to radiation. For this reason, radiographs are normally not taken on pregnant women unless there is an emergency that requires it. Especially with pregnant women it is far better to err on the side of safety where possible. The use of a lead apron would make it possible and relatively safe, but where pregnancy only lasts a relatively short time, the usual decision is to wait until after the baby has been delivered and be totally safe.
____________________________________________________
Periodontal Disease
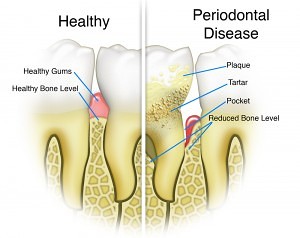
Periodontal or as it is often more commonly called, gum disease, is actually the cause of more lost teeth than cavities. It is the most common human disease there is, and it is caused by dental plaque. We have talked a little bit about dental plaque in the sections on brushing, flossing, and cavities. Plaque is a thin sticky film of bacteria, food debris and bacterial products that forms on the surface of the teeth and gums. If you clean it off, the bacteria starts to settle on the teeth right away and begin forming new layers of plaque. For periodontal disease as well as cavities, prevention is a continuous process of removing the plaque on an ongoing basis through brushing a number of times through the day and flossing once a day.
The damage that is done is accomplished through the destruction of the tissues (bone, gums, ligament) that support or hold the teeth in place so that the tooth gets looser over time and eventually the damage to the gums and bones creates a deeper hole or space around the tooth that breeds bacteria at a greater and greater rate and leads to an abscess. You can get abscesses from cavities as well but the mechanism is different and they don’t always lead to the loss of the tooth.
Periodontal or gum disease is usually not a continuous steady process that affects all the gums equally. Instead it usually progresses in fits and starts and in some areas of the mouth more than others. Any areas that are more difficult to keep the plaque cleaned off are more likely to get periodontal disease progressing. You can get active disease in the gums and supporting structures on one area of a tooth and have another area of the same tooth be fine, just due to differences in keeping the plaque cleaned off. Eventually though, periodontal disease in one area of a tooth will jeopardize the whole tooth. If you picture digging a hole in sand you notice that the deeper you dig, the wider the hole gets. It is similar with periodontal disease, the deeper the area of bone loss, the more it widens out around the tooth.
The treatment and prevention of periodontal/gum disease is the primary function of a dental hygienist. People often think of them as merely cleaning teeth as part of a cosmetic function but instead they are a major component of the treatment and prevention of periodontal disease. You yourselves and what you do for home care is the other biggest component.
Dental plaque that has been there for a while begins to pick up mineral from your saliva and become a hard rough substance called calculus or tartar. The rough surface of the calculus traps more bacteria and leads to even more plaque formation. The porous nature of the calculus also absorbs and holds bacterial secretions that further damage the gums, ligaments and bone. Once the calculus forms it is too hard for a toothbrush or floss to remove. It can also form in areas between the tooth and gum (pockets) that are too deep for the brush and floss to reach. Removing this hard calculus and getting down to areas that you can’t reach on your own are what your hygienist is doing. The polishing that many people associate with a dental cleaning is often only the last stage of a “cleaning” that is much more heavy duty and much more health related than a cosmetic polish.
Periodontal/gum disease has varying levels of severity and progression. Some early stages can be reversed and damage repaired. Once bone has been lost however, it is normally lost forever and the best you can look at doing at that point is trying to prevent the bone loss from getting worse. Remember that periodontal/gum disease does not progress at an equal rate throughout your whole mouth. You can easily have areas where permanent bone loss has occurred and other areas where the bone and gums are in relatively good condition.
The bone loss and destruction of the supporting tissues of the tooth seen in periodontal/gum disease is not caused directly by the bacteria in plaque. It is caused by your body’s immune system causing an inflammation response to the bacteria. Possibly hair splitting as the bacteria is the initial stimulus, but it means changes in your bodies overall inflammation levels and immune system can have effects on the severity of periodontal/gum disease.
There are variations in how prone people are to periodontal disease. The differences come from a number of factors including, plaque levels due to level of home care, genetic factors, anatomical differences, systemic illnesses like diabetes, and diet to name a few.
There have been links noted in research between periodontal/gum disease and heart disease. More research is needed but this link is probably not a matter of periodontal disease causing heart disease but more that factors influencing inflammation in the blood vessels and tissues, and leading to heart disease, affect the whole body and not just the heart. Nutritional factors which increase inflammation in the body and blood vessels such as higher levels of meat and dairy consumption could play a factor in making gum disease worse, along with the heart.
_____________________________________________________________
Pregnancy and Dental Care

With pregnancy there are a number of dental issues. You hear various stories that the baby will take calcium out of your teeth and cause you to get cavities or lose teeth. This is not true. While a growing fetus needs calcium, it will never come from the mother’s teeth.
It is possible to get more cavities when you are pregnant but they are normally due to indirect causes. For example, if you have problems with morning sickness and nausea you tend to gag more easily and may not get the brush as far back as usual or be flossing the teeth at the back of your mouth as much. You also tend to get food cravings that alter your normal diet. As well, you normally don’t get x-rays taken during pregnancy and this may allow a cavity more time to develop before it is discovered.
One dental change that does occur with pregnancy is that the changes in your body’s hormones cause your gums to have a greater inflammatory response to any dental plaque or bacteria that is present in the mouth. This means that periodontal/gum disease will be worse and your gums will be more prone to bleeding. This is an exaggerated response to the bacteria that is there so it is not seen if your oral care is such that the plaque and bacteria is controlled adequately, but the threshold levels for seeing symptoms is much lower.
This increased inflammation of the gums and bleeding is normally a temporary problem and disappears after the pregnancy is over and hormone levels return to normal. It is still an indication that brushing and flossing is not as good as it could be however.
As far as treatment goes during pregnancy, normally an attempt is made to do little or no, invasive procedures. The usual philosophy is that while it may be totally safe, don’t take any unnecessary risks with a pregnancy. X-rays are usually not done except in case of an emergency.
The most critical time is during the first trimester. Things like fillings, etc., are normally delayed until after the first trimester or even until after the baby is born if the problem does not seem overly time critical. If fillings etc. are done, the question often comes up of whether or not to use local anaesthetic (freezing). Following the principle of avoiding any risk to the unborn fetus, local anaesthetic may not be used but this must be balanced with the stress to the mother and therefore the fetus of not using local anaesthetic which may be much worse. Again, the best choice is often to delay treatment until after the baby is born if possible.
Dental cleanings for most pregnant mothers are non-invasive enough to be of no concern and are even beneficial in helping to control the increased inflammation of the gums that results from the hormonal changes.
__________________________________________________
Dental Care for Your Infant or Toddler

Beginning dental care early is important for your child’s health. Many parents wonder if it really matters as the baby teeth are going to fall out anyway. It does matter. Healthy baby teeth help children eat and speak clearly. Baby teeth guide permanent adult teeth into the proper position. Heavy decay or the premature loss of baby teeth can result in problems with the position of permanent teeth that requires orthodontics to correct. Cavities can lead to pain and infections if not treated. Also, some baby teeth are not replaced by permanent teeth until the age of 12 or 13, so some of them are there for a long time. Dental care includes cleaning your baby’s gums before the teeth come into the mouth.
Cavities are caused by a combination of factors including the bacteria that normally reside in the mouth. Bacteria can be passed to your baby from other family members through saliva. If family members have healthy teeth, they are less likely to transmit cavity causing bacteria to the baby.
You can reduce the chance of passing cavity causing bacteria to your baby. Do not share toothbrushes, lick soothers to clean them, and avoid feeding your baby with the same spoon that has been in your mouth.
How can tooth decay be prevented?
Good dental care includes cleaning and checking your child’s teeth and mouth every day. Lift the lip so you can see along the gum line when cleaning and look for white or brown spots which may be early signs of tooth decay.
Gently clean your baby’s mouth using a soft baby toothbrush or wet face cloth. When teeth start to come in, use a toothbrush with a smear of fluoride toothpaste the size of a grain of rice. Brush your child’s teeth in the morning and especially at bedtime. As small children often end up swallowing more toothpaste than an older child or adult would, using smaller amounts of toothpaste is advised. Especially toothpaste containing fluoride as the levels in toothpaste are meant for topical use and not meant to be swallowed.
Children’s toothpaste without fluoride is available and while the usual recommendation is to use a toothpaste with fluoride, for younger children a toothpaste without fluoride is useful to help prevent your child swallowing too much fluoride. While the results of young children swallowing fluoride toothpaste are normally limited to small whitish discolourations on the teeth, it is best to minimize it.
Once your child turns 3, brush your child’s teeth using a “pea-sized” amount of fluoride toothpaste on a soft child’s toothbrush.
When will my child get teeth?
Children have their own schedule for teething. Most children begin teething at about 6 months of age. Your child should have all of their first set of teeth – or “baby” teeth – by 3 years of age. The bottom front teeth usually appear first, followed by the top front teeth. In total, 20 teeth should appear – 10 in the top jaw and 10 in the bottom jaw. The section on “Tooth Eruption” shows average times that the different teeth come into the mouth.
Note: Tooth development can vary and the charts provides a general guide only. In most cases, infants have some teeth by their first birthday but some children are born with teeth. Most kids have lost all their baby teeth by the time they go to high school. If you have any questions or concerns about the development of your child’s teeth, speak to your dentist.
How can I comfort my baby when they are teething?
Teething may cause some discomfort, making your baby fussy. Your baby may feel better if allowed to chew on a clean, chilled teething ring, teething toy, or clean wet face cloth. Teething cookies or biscuits are not a good choice because these can stick to your baby’s teeth and cause tooth decay.
Check with your doctor, dentist or health care provider before using teething ointments, gels or tablets, or any other teething items.
Teething itself does not cause fevers. If your baby has a fever or diarrhea while teething, treat it as you would at any other time and consult with your physician if need be. What often happens is that the antibodies the child received from the mother before childbirth are wearing off and the child is still developing their own. This temporary lowering of their immune system makes them more prone to fevers and diarrhea. The timing for this is often the same as when a child first begins to get teeth but the two are not normally related other than by coincidence.
Can the food my child eats cause tooth decay?
Eating sugary foods or drinks or eating snacks all day long may increase the risk of tooth decay.
Cavity causing bacteria in the mouth break down starches and sugars in foods which produces acid that cause tooth decay. Fruit juice, sweetened tea, soft drinks, all types of milk, and formula contain sugars that can cause tooth decay if in contact with teeth for long periods of time. Tooth decay can develop when a child uses a bottle with these liquids for long periods, especially during rest or sleep times. Your child is also at increased risk for tooth decay if they continually sip anything other than plain water from a bottle, drink box, or sippy cup.
Water will not harm the teeth. Water is a good choice between regular feeding times and for thirst. Introduce your baby to using a cup between 6 and 9 months of age.
What about soothers or pacifiers?
Soothers or pacifiers are sometimes given to babies during rest, sleep or other times. If you choose to give your baby a soother, here are a few tips:
- ensure that breastfeeding is well established;
- choose the right size soother for your baby’s mouth;
- check the soother nipple often – throw it away if it is sticky, cracked or torn;
- keep the soother clean;
- avoid dipping the soother in honey or other sweet substances that can cause tooth decay; and
- by age 1 or 2, if a soother is used, limit use to nap time or bedtime.
- Soothers or pacifiers are not recommended once all baby teeth have grown in, usually when your child is about 3 years old. After this age, regular use of a soother may affect the child’s speech and language development. Parents can start to “wean” children off the soother as soon as possible.
Can fluoride help stop tooth decay?
The Canadian Dental and Medical Associations recommend fluoride for preventing tooth decay for people of all ages. Fluoride is a proven, effective and low-cost way to help prevent cavities. Fluoride helps make tooth enamel more able to resist the acids produced by oral bacteria. Most children will get enough fluoride from using a small amount of fluoride toothpaste twice a day. Some toothpastes do not have fluoride. Always check the label.
If you are unsure if your water supply contains fluoride, call your local public health unit. Municipal water supplies often have fluoride added and even natural well water may have fluoride in some cases. You don’t know for sure unless you check.
Your dentist may recommend additional fluoride for your child.
When should my child go to the dentist?
Advice on this varies depending on which authority you ask. Our office’s usual advice for most kids is that they start being seen at age 3. They should always be seen sooner if you notice any problems with their teeth before that. It is around this age for most children that they tend to exhibit the level of cooperation needed to make a meaningful assessment of their oral health. As in all things, there are exceptions to this tendency. Your child’s first dental visit is a good time to discuss daily dental care, fluoride, and eating habits. If you have a concern about your infant’s or toddler’s teeth, make an appointment to see your dentist.
__________________________________________________
Tooth Eruption
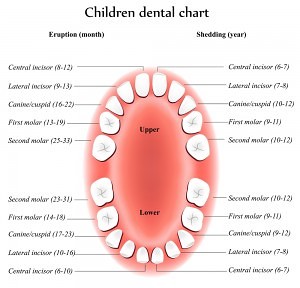
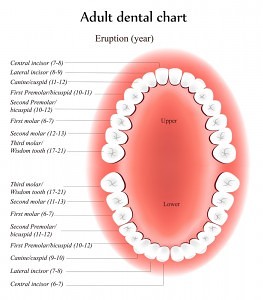
Teeth form inside the bone of the upper and lower jaws and then “erupt” or move through the bone and gum tissue to enter the mouth. This happens initially with primary or “baby” teeth and again with permanent or “adult” teeth. They do this by stimulating cells ahead of them to dissolve away the bone in their way so that they can move ahead. The erupting tooth also stimulates the cells behind it to lay down new bone after it as it moves through the bone.
The charts above show the usual times that this happens. These times are averages and can vary quite a bit between different people. If a person has their primary/baby teeth come in later than the average, their permanent/adult teeth will usually come in later as well.
When the adult teeth erupt, the ones that form under the primary or baby teeth will move into the mouth by dissolving both the bone and the root of the tooth ahead of them. If you look at a baby tooth that has fallen out you may wonder how it managed to stay in the mouth in the first place, but what you are seeing is the top or crown of the tooth after the roots have been dissolved away.
It is possible for a tooth to form in an incorrect position and to erupt in such a way that it destroys part of a tooth that it shouldn’t. You will see this occasionally with a third molar or “wisdom tooth”. In some cases this can result in the loss of a permanent tooth.
In other cases the erupting tooth does not dissolve the tooth ahead of it and in this case it gets blocked and unable to enter the mouth.
__________________________________________________________
Nursing Bottle Syndrome

Nursing bottle syndrome is easily preventable. It is usually caused by putting young children to bed at night with a bottle containing milk, formula, juice or some other liquid containing sugars. Whether it is natural sugars like those found in milk or added sugar as in many juices, it doesn’t matter, both can cause problems.
At night the natural saliva flow in the mouth slows down and with the above types of liquids the front teeth are bathed in lots of sugar. The two events work together to cause a huge increase in bacterial activity producing cavity causing acids.
The results are similar to the above picture or in many cases even worse. Extensive damage from cavities occurs in the child’s teeth and they can become abscessed and painful as well. The result is a requirement for extensive dental treatment and in some cases even extraction of the affected teeth.
You can get similar results by dipping a pacifier in something sweet like honey and giving it to the child on a repeated basis as well.
A much better choice if you are going to put your child to bed with a bottle at night is to use water in the bottle. If there are no sugars, there is no nursing bottle syndrome.
_______________________________________________________
Hazards of Thumbsucking

Thumbsucking is a very common habit among younger children. As long as it stops early enough it will not cause problems.
What will begin to happen as the child grows though is that if will affect the way in which the actual bones of the face grow. The repeated sucking action on the thumb and having the thumb positioned between the front teeth begins to cause a situation where the bone of the upper jaw deforms to allow room for the thumb to sit between the upper and lower front teeth.
You begin to notice a large noticeable gap from the front teeth splaying forward and the bone itself reshaping to make room for the thumb. There is a lot of growth and development going on with young children and their bones are much more plastic and adaptable.
If the thumbsucking stops early enough, these changes in the bone and teeth will correct on their own. If it is left too long they become permanent and require orthodontics and sometimes surgery to correct adequately.
There are a number of ways to try and stop the thumbsucking habit. Sometimes encouragement and explanations can lead the child to quit.
Bad tasting liquids can be painted on the thumb to discourage the habit but these seldom work. The children will often continue to suck their thumbs despite the bad taste.
Substituting a soother for the thumb can sometimes work as a transition or stepping stone to breaking the habit. Using a soother for too long can cause the same problems as thumbsucking but the soother is usually smaller than a thumb and causes less deformation. More importantly, children will tend to find a soother habit easier to break. As they get older, the soothers are seen as being more and more juvenile and inappropriate by other children and peer pressure tends to break the habit.
Another method which has almost perfect success is to have your dentist or an orthodontist fabricate and install a thumbsucking appliance. This appliance is attached to the teeth using a dental cement so the child cannot remove it. They are designed to leak air so the child cannot get the soothing sucking sensation they are used to.
The other behavioural solutions are normally tried first and an appliance is often only made as a last resort. If your dentist is noticing a problem with how the teeth and bones are developing due to thumbsucking, they will usually suggest either parents try behavioral solutions at home or arrange to have an appliance made and inserted. Once the habit has ceased the appliance is removed at a later date.
_____________________________________________________
My Child is Getting a Second Row of Teeth!?!

It is not uncommon for mothers to bring their children to the dentist because they are concerned to notice a situation like the one in the photo above. For many children this is a normal temporary phase in the eruption of their permanent teeth, especially on the lower front teeth. For others this is the beginning of a problem that may need orthodontics to solve. In either case it is not cause for panic and it will often take some time to tell which will be the case.
In the section on eruption of teeth it was explained how adult teeth will move into the mouth, dissolving away bone and baby tooth roots ahead of them. They can still be redirected slightly to follow paths of least resistance. Also, there is a certain randomness as to how a tooth is turned or oriented once it comes into the mouth, but once there, the tongue, lips and cheeks place forces that assist in guiding them to where they should be and rotating them to how they should be oriented.
If you look at the picture above you can see that the adult teeth are coming in behind the baby lower front teeth. It can be easily seen that the two adult teeth are wider than the two baby teeth they are replacing. They can’t physically fit in the space provided by their two baby counterparts. This lack of space due to the different sizes in the baby and permanent front teeth will sometimes result in the adult tooth causing more than one baby tooth to fall out to create the space it needs. Often though, it will take a path of lesser resistance and erupt behind the lower front tooth. What frequently happens then is that as the adult tooth erupts further into the mouth there becomes more tooth for the tongue to press against. This pressure then causes the adult tooth to tip forward into the space it should be. Quite often the corresponding baby tooth will fall out on its own from the adult tooth moving forward, it just takes a bit of time. In some cases a portion of the baby tooth will be left hanging on and need to be extracted, but the small remaining portion is usually not a difficult extraction.
There is no harm in taking your child to the dentist to have them checked as it may cause the dentist to pay closer attention to the eruption process and possibly head off potential problems a bit sooner. Quite often though the dentist’s advice will be to give it some time and see if the problem corrects on its own first, and most of them will.
__________________________________________________
Sealants

Dental sealants are a preventive measure that is helpful for some patients.
If you feel the tops of your back teeth with your tongue you can feel several hills and valleys on your teeth. At the bottom of the valleys there are a variety of grooves and fissures on the chewing surfaces of the teeth. These grooves are related to how the teeth actually form initially.
When these grooves and fissures in the teeth are deep and narrow, you are more prone to getting cavities in them. They create areas that you cannot get into to clean out the plaque. The bacteria in dental plaque can easily grow in areas far too narrow for a toothbrush to get into and can happily sit there eating sugars and producing acids.
If your small grooves and fissures are very shallow and wide, you don’t have this problem. It does not mean you can’t get cavities, it just means that cleaning the plaque off, is much easier in those areas.
Sealants are the final product of a process where a liquid plastic is flowed into these narrow, deep grooves and bonded and hardened to fill in, and eliminate them. It is common for a dentist to recommend sealants on patients that have deeper grooves. Some dentists will even recommend sealants for all posterior adult teeth. There is no drilling, no freezing and the sealant material is usually set with a bright curing light as seen in the picture above. All in all, they are usually a simple, non-traumatic, minimally invasive, form of preventive treatment.
In theory they are a great solution. In practice, they can be a very good one. As with any procedure they are not perfect. As a preventive measure, they are best considered on patients in groups. You will find that a group of patients with sealants will have fewer cavities than a group of patients without sealants. Having sealants on an individual patient does not mean they won’t get a cavity in the area the sealant was placed and they are still just as prone to cavities on other areas of the teeth. Your likelihood of getting a cavity in an area a sealant is placed is statistically less, just not guaranteed less.
There some possible drawbacks to sealants. They can be lost with wear and need touched up or replaced with time. Care should be taken that sealants are not placed after a cavity has already started. In the case of deep narrow grooves, it can be very difficult to detect cavities in their early stages. Insurance companies usually will only cover the cost of placing sealants during a small window of time for specific teeth. Often two years from the usual time of eruption. If your child’s teeth erupt at a slower rate than average, this can cause issues with the insurance coverage.
Some arguments can be made that the cost of sealants does not justify the possible percentage reduction in cavities but they are less expensive than fillings and especially on children that have deep, narrow grooves in the shape of their teeth and/or are more cavity prone, they can be an excellent option that is easily worth the cost.
_____________________________________________________
What to Do if a Tooth Gets Knocked Out

If you or a child have an accident and have a tooth knocked out, what do you do? It might be a single tooth or more than one tooth and it could be a baby tooth or a permanent tooth.
The first concern is whether you or the child lost consciousness. If so, you should go to an emergency room to be checked for the possibility of concussion or internal bleeding to the brain. Let them know about the tooth or teeth as well as their treatment may be time sensitive but a loss of consciousness is a greater concern.
Assuming there was no loss of consciousness, contact your dental office.
Often a baby teeth is of less concern as it is a tooth that will normally be replaced by a permanent tooth later. This is not always the case as some people have a situation where they don’t have a permanent tooth below the baby tooth and the baby tooth is the only one they will get. This is not the usual case but it is not rare. Either way it should be checked by a dentist. Even if the tooth is not saveable, there may be other damage that you can’t see from the trauma that caused the tooth to be knocked out.
The tooth or teeth that are knocked out may be able to be saved. First find the tooth that was knocked out. Normally the best way to clean it is to suck it. Your own saliva is the best thing to put on the tooth, much better than milk or water.
Once the tooth has been cleaned, try and push it back into the socket. If you can get it to go back in, great. You still will have to see a dentist as soon as possible but it increases the odds of the tooth being saved.
If you can’t get it to go back into the socket keep it under your tongue or inside the cheek being very careful to not swallow it, and get to a dentist as soon as possible.
The dentist, after getting a medical history and history of the accident will probably take an x-ray to check for other damage in the area. A force large enough to knock out a tooth can easily fracture bone or tooth roots on other adjacent teeth.
There will be three main options as to how the dentist may proceed.
- Leave the tooth out and after healing look at replacing it with a bridge, implant or partial denture.
- Use the tooth that was knocked out to make a temporary replacement, and look at replacing it later with a bridge, implant or partial denture.
- Try and put the tooth that was knocked out back in place and stabilize it so that it is held in place. This is what you are hoping for by keeping the tooth and bringing it to the dentist as soon as possible. Success of keeping the tooth is not guaranteed, but if successful it is usually a better option than the first two listed above. It is often worth the attempt as if it is not successful, you can still look at doing the options listed above. Once the tooth is put back into place, the dentist will have to monitor it for the next year or so.
As a final note, wearing a mouthguard for sports and other highly physical activity is highly recommended to try and prevent the trauma to the teeth in the first place. You can still have other non-sports related accidents but at least you are helping to protect against the riskier ones.
__________________________________________________
Wisdom Teeth

Wisdom teeth are the common name for permanent third molars. On your permanent or adult teeth, if you look in the back of your mouth and see the large molar tooth (the one with the four or five bumps on top) closest to the front of your mouth, that is the first permanent molar. The large tooth behind that is the second permanent molar and the one behind that (if you have it or if it has erupted into the mouth) is the third permanent molar or wisdom tooth.
They are normally the last tooth to erupt or come into the mouth, usually around age 17 – 21. They are a variable tooth in many ways. Not everyone even has wisdom teeth. Most people have four of them (one on each side on both the top and bottom) but some people have three, two, one, or none of them at all. Some people even have more than four (they are technically supernumerary or extra teeth but in that area of the mouth are usually thought of and treated as extra wisdom teeth for practical purposes).
If a wisdom tooth erupts or comes into the mouth normally and in a straight upright position and you have enough room for it without having part of the top of it covered by gum tissue then it is just another tooth and nobody cares about them other than as being more difficult to keep clean from being so far back in the mouth. The sizes of teeth in general can vary from person to person as can the physical size of the bones in the jaws. If you have larger jaw size and smaller teeth you usually have lots of room for the wisdom teeth to come in. If you have larger teeth and smaller jaw size, you usually don’t have space.
Where difficulties or concerns arise are if a wisdom tooth does not erupt but stays under the gum and bone, if it comes in only part way, or if it comes in crookedly or on its side. The most common problem seen with wisdom teeth occurs when they erupt only partly into the mouth. This leaves a situation where there is a flap or pouch of gum tissue over part of the tooth that traps bacteria and cannot be cleaned adequately and causes recurring gum infections or abscesses. On a tooth that erupts normally this can occur as well but it is only a temporary problem that disappears once the tooth fully erupts (teething is an example of this on other teeth). If there is not enough space, the tooth physically can’t erupt further and the problem of the gum tissue over part of the tooth becomes permanent. Surgical attempts to remove this gum tissue have been tried in the past to eliminate the problem and keep the wisdom tooth but the gum tissue will usually grow back and the problem return.
You can get other problems develop with wisdom teeth as well. In the section on tooth eruption it was mentioned that teeth move through the bone by activating cells ahead of them to dissolve away bone and tooth roots (this is how adult teeth erupt and get rid of the baby tooth and bone above them). If a wisdom tooth is tipped forward or is on its side you will sometimes see them begin to destroy part of the root on one of the other teeth.
Teeth that don’t erupt but stay in the bone are more prone to cysts forming around them.
For all of the reasons above and more, the decision of whether or not to recommend extracting the wisdom teeth can vary. A judgement is made on whether it looks like there will be enough room for them and whether they will come in straight, etc.. There are also potential complications with the surgery to extract them. The roots of the wisdom teeth can be in very close proximity to large nerves and blood vessels and the surgery can have a risk of temporary or permanent damage to nerves in that area. If they are extracted, healing is normally better on younger individuals than on older individuals and this has to be considered. All of these factors and more are weighed in the decision of whether or not to recommend the extraction of wisdom teeth.
It is important to realize that each individual wisdom tooth is an individual case. They are often referred to as a set and but you may have three out of four wisdom teeth come in fine and have one positioned to have problems or during extraction, the surgery can be easy with few complications or more difficult based on each individual tooth. One surgical site may have minimal problems with pain or healing and a different one have more pain during healing. It varies with each specific tooth.
For extractions wisdom teeth are usually done as a single procedure to extract all of them at once. This is usually done under sedation of some form. It is often done this way for patient comfort and to make it a single surgical procedure to endure. It does not have to be this way. They can be extracted with just local anaesthesia and they can be extracted one at a time. This can be a matter of patient preference and sometimes of available patient finances. If a patient does not have dental insurance and has difficulty affording the removal of all the wisdom teeth at once under sedation the extractions can be staged to only extract only the ones that are currently bothering the patient at the present time and delay the others until the patient is able to afford it.
The most common preference by patients though is to get them all done at once under sedation.
Since some wisdom teeth can be more complicated to remove or because of a wish to have the sedation, they are often referred by general dentists to a specialist for removal.
________________________________________________________
Loose Dentures

Denture wearers can suffer from loose dentures for a variety of reasons. If they are new dentures and an older pair of dentures do not currently feel loose then the new dentures probably need adjusted by your dentist or denturist. If you are making this comparison with how an old set of dentures used to fit and how a new set currently fit, this may not be the case, as there may have been changes in your mouth since the earlier set were made. Either way it does not hurt to have your dentist or denturist check them.
One of the larger changes that occur are that the actual shape of the bone supporting the dentures changes over time. Structurally, much of the bone in your jaws is present to support the teeth. Once the teeth are gone your body begins to remodel the bone and actually dissolves away bone that used to support teeth that are not longer there. What is left is the basal bone which does not project up into the mouth as much and therefore does not give as much support to dentures. The more bone that is lost, the looser your dentures will fit.
You can see this process at work on areas where even a single tooth is lost. You will notice over time that bone in the area of the lost tooth becomes much narrower and much lower than the adjacent teeth. As more teeth are lost, this same process occurs over a wider area. This means that you will periodically need dentures adjusted, relined, or rebased, or even have a new set made to keep them fitting well.
If the artificial teeth on your denture are not too badly worn then you may be able to have just a reline or rebase done. These are less expensive than a new denture and both alter the internal shape of the denture to conform to the way the bone has changed shape in your mouth.
Large amounts of general weight loss can also cause dentures to become looser. While the bone does not change, the amount of soft tissue reduces and can cause dentures to be less snug the same as your clothes do.
Having less saliva in the mouth can cause dentures to fit looser with less suction as well. You may have noticed that suction cups of any type stick better if they are moistened first. The moisture aids in getting a better seal. This lowering of saliva levels in the mouth can happen for a variety of reasons. As we age, we naturally produce less saliva. Some medical conditions can cause a drastic lessening of saliva and prescription drugs often have the side effect of decreasing saliva production.
With any noticing of looseness on dentures your first course of action should be to check with your dentist or denturist to see if anything can be done by altering your existing dentures or making a new set. If this fails to solve the problem totally, resorting to a denture adhesive of some sort may be a suitable option for you. Denture adhesives come in a variety of forms such as powders, creams, or strips and it is a matter of choosing one that seems to work best for you and your preferences.
A final possible option is to consider having dental implants placed into the bone. These are then used to anchor your dentures in place. There are different methods of using implants to anchor dentures and usually one can be found that will work for you.
It is worth noting that while looseness can occur with any denture, it is more commonly a problem with lower complete dentures. Most people assume it would be the upper dentures that would be the problem but this is usually not the case. If you look at the dentures in the photo above, the one that looks like a horseshoe shape is the lower. The upper denture is of a shape that better allows more tissue coverage and more suction. Lower dentures have to allow room for the tongue which is an extremely strong muscle that tends to move the lower denture wherever it wants. With new dentures, patients normally find the lower denture takes more to adjust to, and take more time to get the knack of how they work best.
_____________________________________________________
Diabetes and Oral Health

If you have diabetes, whether it is type 1 or type 2, you are more prone to a wide range of medical complications of a general nature. The mouth is just another part of your body and is not immune to these complications. The general complications of diabetes do lead to certain specific dental problems. The main oral complications of diabetes are infections and dry mouth. Together they can lead to tooth decay, periodontal/gum disease and delayed healing after surgery.
Dry Mouth
Xerostomia is defined by a state of dryness in the mouth caused by a lack of saliva, or a lack of saliva production by the salivary glands. There can be a variety of causes of xerostomia, but diabetes is one of them. If you are diabetic, the increase of sugar in your saliva leads to a decrease in the quantity of your saliva in your mouth.
Suffering from dry mouth can lead to complications such as cavities for two reasons. Saliva contributes to a natural cleaning of teeth by helping to flush away the bacteria and acids produced by the bacteria in dental plaque. As well, the extra sugar in the saliva of diabetics acts as another source of sugar for cavity causing bacteria to convert to acids. Moreover, a lack of moisture can also lead to the development of ulcers, fungal infections and difficulty to wear removable dentures. One of the best ways to treat xerostomia is to drink water more frequently. But in some more serious cases, drug therapy is recommended.
Another consequence of xerostomia can be burning mouth syndrome, which is described as a burning sensation on the tongue and other parts of the mouth. It is a painful situation that can be frustrating for the person that has it. It can sometimes be felt like putting very hot liquid into your mouth. Burning mouth syndrome also can have a number of causes but if it is caused uniquely by xerostomia, it should be treated as described above.
Periodontal Disease
Periodontal/gum disease, is a chronic bacterial infection that occurs around the teeth and can eventually lead to the destruction of the bone and tissue supporting the teeth and holding them in place. If it is not treated, your teeth can eventually get loose and even be lost.
Periodontal/gum diseases tends to be more severe among people who have diabetes because diabetes lowers the ability to resist infection and slows healing. An infection such as periodontitis may also cause your blood sugar level to rise, which makes your diabetes more difficult to control. Preventing and treating periodontitis can help improve blood sugar control.
It is very important to check the condition of your gums on a regular basis, and treat periodontal disease if you are diabetic.
Hygiene and Dental Treatment
Because diabetes makes teeth and gums more susceptible to certain diseases, it is important to give special attention to your oral care, both at home with excellent brushing and flossing and by your dental office.
Here is a summary of advice offered to diabetics:
- Make a commitment to managing your diabetes. Monitor your blood sugar level, and follow your doctor’s instructions for keeping your blood sugar level within your target range. The better you control your blood sugar level, the less likely you are to develop gingivitis and other dental problems at a higher than normal rate.
- With few exceptions, people with diabetes can receive dental treatment as anyone normally could. Dentists often recommend short dental appointments taken preferably in the morning. You must also take your meals and your insulin as you normally do without any changes to avoid hypoglycemia (low blood sugar). The common signs of hypoglycemia are loss of coordination, blurry vision, palpitations, rapid heart rate, sweating and shaking. It would be advised to bring a source of emergency sugar in some form to dental appointments in case you become hypoglycemic.
- If tooth extraction or any kind of surgery is necessary, you must expect a longer healing period and a good follow-up with your oral surgeon or general dentist.
- Any surgery or extractions must only be accomplished if the level of blood sugar is well controlled. Otherwise, you must postpone the treatment, unless there is an infection or an abscess, which should then be treated immediately.
___________________________________________________
What To Do After a Tooth is Extracted

What to do after a dental extraction can be broken into two general time frames; right after the extraction, and long term. Whether it is a single tooth is extracted, or several teeth, the same general principles will apply.
Right after a tooth is extracted you have a hole in the gums and bone where the roots of the tooth used to be. Immediately after the extraction, any bleeding from the tooth socket is controlled with pressure. This is usually done by using one or more pieces of damp cotton, either in the form of small gauze pads or cotton rolls, depending on what fits into the space better. These are usually held in place by biting down on them. The dentist or their assistant will usually give instructions as to how long pressure with the gauze should be applied before it is removed. The amount of time pressure is applied can vary from about 20 – 45 minutes depending on a variety of factors that may affect the amount of bleeding. The pressure on the cotton is just meant to control any bleeding until your body’s clotting mechanism causes it to stop.
Stitches may or may not have been placed. Stitches can be used to hold the tissue together and also to help control bleeding. Whether or not they are used will depend on what exactly was done during the extraction and the anatomy of the situation. In many situations they are not required.
If stitches were used they fall under two main types; 1) those that will dissolve on their own and 2) those that have to be removed at a later appointment. If they are the type that dissolve on their own, the part that is in the tissue itself will be destroyed and absorbed by your body, leaving the knot and the rest of the stitches outside the body to get loose and fall out.
Once the blood clot has formed and the cotton has been removed, for that day, extra care must be taken to not disturb the blood clot. Hot drinks should be avoided in the area so the clot is not washed out. Strenuous activity is to be avoided to prevent a raising of your blood pressure and causing further bleeding. Smoking is to be avoided to prevent smoke from getting into the healing socket. Rinsing with mouthwashes or in general should be avoided that day to help prevent the blood clot being dislodged.
Any pain medication that is prescribed or recommended is often best taken before the local anaesthetic (freezing) comes out. This eases the transition from freezing to no freezing and helps prevent a situation where you are in pain and wishing the pain medication would work much faster.
If you do have any problems with the extraction site bleeding again, take some of the extra gauze or cotton rolls that the dental office usually gives you and dampen it with water from the tap. If the cotton is moist the blood clot won’t stick to it as it forms. If you use dry cotton the clot sticks to the gauze and when you remove it, the clot often comes with it.
If you don’t have any cotton from the dental office or have used it all, tea bags make a great substitute and the tannic acid in the tea also helps promote blood clotting. The tea bag should also be dampened and used wet. Again you bite down on the cotton or tea bag for 20 – 45 minutes.
With extractions for immediate dentures, the denture itself will perform the same function as the cotton or tea bag and is used instead. Often instructions are given to not remove the immediate dentures until the next day. This is done for two reasons; one, the denture covers the wound site until the blood clot is fully organized and two, if there is any swelling at the extraction site it will conform to the shape of the denture. If you take the denture out too early and swelling occurs, you may not be able to get the denture back in until the swelling goes down.
Starting the day after the extraction the instructions change. The blood clot has matured somewhat and is not as prone to being lost. You can still dislodge it and start things bleeding again but it takes much more. Gentle rinses with warm salt water (a teaspoon of table salt in a glass of warm water) should be used to rinse the extraction area gently, a number of times through the day. You continue this until you can clean the area normally with a brush and floss. It is important to keep the area clean and until it heals further you should not use a tooth brush in the area. The more it heals the more you can get into the area with a brush and floss, but initially you need to rely on rinsing. In some cases the dentist may give you an antibiotic mouth rinse to use instead of the salt water.
Pain medication should be continued until you no longer need it. As it heals you can normally cut back on the dosage and frequency.
The levels of pain with an extraction can vary a lot depending on how difficult the tooth was to remove. More complicated extractions result in more damage to the bone and gums around where the roots of the tooth used to be. The more damage, the more post-operative discomfort there tends to be.
If after the extraction the pain or discomfort levels is decreasing, that is normal. If you find the pain or discomfort levels decrease for a few days and then start to increase, check back with your dentist as that is usually a sign that the extraction site has become infected. The extraction site is basically an open wound and the inside of the mouth has lots of bacteria present so an infection is quite possible. The infection can be of a typical kind that clears up well with antibiotics or you can get something called “dry socket”. This is still an infection but of a particular type. With dry socket the bacteria causing the infection attack the blood clot itself and destroy it. This leaves the bare bone of the extraction site exposed and painful. It will heal over on its own, it is just very uncomfortable while it does. This type of infection does not respond to antibiotics well as once the blood clot is destroyed the damage is done. There are a variety of treatments your dentist can do that can drastically decrease the discomfort of dry socket if it does occur.
Another complication with extraction that is fairly common is for small pieces of bone to work their way to the surface of the extraction site. Small areas of bone may have the blood supply to them damaged during the extraction and these small areas die and then the body expels them by working them to the surface. You will feel them with your tongue after the extraction and they may need to be removed but it is usually a minor procedure.
Longer term you may have to make some decisions about what to do with the space where a tooth used to be. Viable options can include doing nothing, replacing the tooth with a denture of some sort, replacing the tooth with a bridge, replacing the tooth with an implant or some combination of these different treatments. The option of doing nothing about replacing the extracted tooth can be the best one for some situations but this is by no means true in all cases as losing a tooth usually leads to the other teeth in the area and opposing it, shifting in position and angulation. There are a number of possible complications that can occur from extracting a tooth and leaving the space non-restored.
A number of factors can affect which of the possible options is best for a specific situation and your dentist can help you by advising you on the pluses and minuses of each option. Some options may be improved by making some changes at the time of the extraction so deciding sooner rather than later is sometimes beneficial. At whatever time you decide though, there are usually options to choose from.
__________________________________________________
Acid Erosion

Tooth enamel is the strongest substance in the human body. This semi-translucent, hard, outer layer of the teeth has an important job: protecting teeth from the daily wear and tear of biting and chewing, as well as temperature extremes from hot or cold foods and drinks. Enamel also guards teeth against the erosive effects of acids and chemicals.
Enamel covers the dentin, a part of the tooth that is not as dense as enamel. When enamel erodes, the dentin loses some of its protection. Then, the microscopic tubes inside the dentin allow hot, cold, or sweet foods to stimulate nerves within the tooth. As a result, you may notice that your teeth have become painfully sensitive to hot or cold foods and drinks and sweets.
Acid erosion or dental erosion is a type of tooth wear caused by acids that are not from cavity causing bacteria. It is the irreversible loss of tooth structure due to acidic chemicals (both natural and added) in foods and other sources. There are a variety of sources for these chemicals with the majority of erosion cases being caused by what we eat and drink.
Soft drinks are a major source, but there are many others. Fruits and fruit juices for example are a major source of acids causing erosion of the teeth but are not usually thought of as they are generally a healthy food source.
In general, foods and drinks with a pH below 5.0–5.7 have been known to trigger dental erosion effects. Examples are orange juice (which contains citric acid) carbonated drinks such as colas (in which the carbonic acid is not the cause of erosion, but citric and phosphoric acid).
Additionally, wine has been shown to erode teeth, with the pH of wine as low as 3.0–3.8. Other culprits are sports drinks, beer, lemonades, and apple juices. Overly frequent ingestion of any of these can lead to possible problems with acid erosion of the teeth. This does not mean to not have things like fruit or fruit juices but to watch the amounts and times of ingestion. Frequency rather than total intake of acidic juices is the greater factor in dental erosion. Infants using feeding bottles containing fruit juices, especially used as a comforter are therefore at greater risk of erosion.
Our body’s production of saliva acts as a buffer, helping to regulate the pH when acidic drinks are ingested. Drinks vary in their resistance to the buffering effect of saliva. Studies show that fruit juices are the most resistant to saliva’s buffering effect, followed by, in order: fruit-based carbonated drinks and flavoured mineral waters, non-fruit-based carbonated drinks, sparkling mineral waters.
Other possible sources of acids include a number of medications such as vitamin C, aspirin and some iron preparations which are acidic and may contribute towards acid erosion.
Dental erosion can also occur when gastric acid from the stomach comes into contact with the teeth. People with eating disorders such as anorexia nervosa or bulimia often suffer from dental erosion. Gastro esophageal reflux disease (GERD) is another culprit. GERD is quite common and an average of 7% of adults experience reflux daily. The main cause of GERD is increased acid production by the stomach. This is not exclusive to adults, as GERD and other gastrointestinal disorders may cause dental erosions in children.
There are many signs of dental erosion, including changes in appearance and sensitivity. One of the physical changes can be the color of teeth. There are two different colors teeth may turn if dental erosion is occurring, the first being a change of color that usually happens on the cutting edge of the central incisors. This causes the cutting edge of the tooth to become transparent.
A second sign is if the tooth gets an increasingly yellowish tint. This occurs because the white enamel has eroded away to reveal the yellowish dentin. A change in shape of the teeth is also a sign of dental erosion. Teeth will begin to appear with a broad rounded concavity, and the gaps between teeth will become larger. There can be evidence of wear on surfaces of teeth not expected to be in contact with one another.
If dental erosion occurs in children, a loss of enamel surface characteristics can occur. Fillings may also appear to be rising out of the tooth, the appearance being caused when the tooth is eroded away leaving only the filling. The teeth may form divots on the chewing surfaces when dental erosion is occurring. This mainly happens on the first, second, and third molars.
One of the most severe signs of dental erosion is cracking, where teeth begin to crack off and become coarse.
Other signs include pain when eating hot, cold, or sweet foods. This pain is due to the enamel having been eroded away, exposing the sensitive dentin.
Many of these signs can have other causes as well so your dentist can diagnose whether the problems seem to be due to dental erosion.
Preventive and management strategies include the following.
- Treating the underlying medical disorder or disease (eg. Bulimia or GERD)
- Modifying the pH of the food or beverage contributing to the problem, by having it with other foods as part of a meal instead of during snacks, or changing lifestyle to avoid the food or beverage.
- Decrease abrasive forces. Use a soft bristled toothbrush and brush gently. No brushing immediately after consuming acidic food and drink as teeth will be softened. Leave at least half an hour of time space. Rinsing with water is better than brushing immediately after consuming acidic foods and drinks. You need to allow time for the teeth to remineralize slightly before brushing.
- Drinking through a straw can help somewhat as it directs the drink farther back in the mouth and bypasses the front teeth.
- Using a remineralizing agent, such as sodium fluoride solution in the form of a fluoride mouthrinse, tablet, or lozenge, immediately before brushing teeth.
- Applying fluoride gels or varnishes to the teeth.
- Fluoride agents work by helping to make the mineral of the tooth more resistant to acids.
__________________________________________________
Your Dental Insurance

Is it covered by my insurance? That is a question we frequently hear in the office. Often our reply is that we don’t know and it depends on your insurance, but we are happy to send an estimate to the insurance company if you would like. Patients may then reply that they have Sun Life or Blue Cross and then expect that we know from that. We know a lot of facts about how your insurance works in general terms but the specifics can vary greatly from person to person and from plan to plan.
For example, maybe you have dental insurance through Great West Life. When Great West Life sold the dental insurance plan to the employer or group that purchased the policy, they negotiated rates for the policy based on what was covered in that particular policy and on what the terms of the coverage were. The insurance company will tailor make a plan for the customer purchasing the plan, drawing on a large basket of different plan options. For example the coverage may or may not cover orthodontic treatment. If it does, the cost of the plan to the purchaser is higher. It can cover crowns and bridges if you want, but the cost of the plan is greater. The specific dental plan is merely a product to the insurance company and they can tailor make it to almost whatever the company or group purchasing that product wants. The company or group purchasing the plan from the insurance company is normally trying to control costs and will add or subtract what is covered to come within a particular budget or cost goal.
All dental insurance plans are definitely not created equally. For example, what percentage of dental expenses are covered? What particular dental treatments are covered or not covered? Are there frequency limitations on things like different types of dental examinations? If the dental expenses are covered, what fee guide is being used as a reference, the current one or one from 3 years ago? Is there an annual maximum on how much the insurance company will cover you for? Is there a deductible amount that the insurance company makes you pay first before they calculate expenses they will cover?
With larger employers the individual dental plans often vary between employee subgroups of that employer as well. Coverage will also often vary between individual contracts so if the contract was just renegotiated with the insurance company or a switch was made to move the coverage to a different insurance provider the specific terms of the insurance coverage also often change.
There are also rules and guidelines negotiated between the various insurance companies on such things as who pays in cases where individuals are covered by more than one dental insurance company.
It is also not just a matter of the specific insurance contract, there are different types of insurance programs. There are private sector plans through an insurance company and government plans. By government plans I don’t mean the plan you may have as a government employee. Those are usually purchased by the government from a private sector insurance company and are also private sector plans.
The type of Government plans I am referring to are created through legislation and includes such plans as Ontario Works, dental coverage for refugees, the Smiles program for children, the Children In Need Of Treatment (CINOT) program and the Non-Insured Health Benefits (NIHB) plan for aboriginal peoples. These plans as mentioned are put in place by the government by legislation to provide dental coverage for various social need situations and have very different rules and guidelines from the private sector plans.
Even within the private sector plans through the dental insurance companies there are some plans that are different than the traditional dental plans most people are familiar with. Two examples of non-standard plans are Preferred Provider Networks and Capitation plans.
In a Preferred Provider Network the private insurance company has approached dentists to join a list of dentists who will provide treatment for members covered by the plan at a discounted rate. The rates are contractually agreed upon between the insurance company and the dentists entering into the agreement. This is done as a cost saving measure for the insurance company. The dentists sign on in an attempt to increase their patient base. From the patients point of view the plan usually gives them the choice to see any dentist they choose but if the dentist is on the list of the insurance company’s “Preferred” providers the insurance company will reimburse a higher percentage of expenses than if you see a dentist not on their list.
A Capitation dental plan is different as well. At their core the capitation plans are a contractual agreement between a dentist and the insurance company where the dentist agrees to perform the treatment covered by the insurance plan that is required for the patients insured in the plan at no cost to the patients. In return the insurance company contractually pays the dentist a set dollar amount per month, every month, for as long as the contract is in place. The coverage only covers the patient if they see the dentist with the contract with the insurance company. As I mentioned this is at the core of the plans. There may be some variations on what coverage, if any, is in place if the patient chooses to not go to the dentist contractually obligated to provide treatment. Basically, the insurance company is transferring the risk of expenses being greater than the fees they charge over to the dentist. The insurance company charges the employer or group taking out the insurance plan a certain amount per member per month and then contractually pays a portion of that to the dentist.
Some employers even do a self-funded direct reimbursement plan and bypass the dental insurance company totally. Stop for a moment and consider that the dental insurance companies try very, very hard in their plan pricing to ensure that the premiums will cover the total cost of reimbursing patients for their dental treatment, plus the insurance company’s administrative, sales and marketing costs and allow for a profit beyond that. It is no surprise then that some companies looking to provide dental benefits to their employees choose to just reimburse the cost of the dental expenses themselves and not pay the extra costs of an insurance company. It means however that they then have to provide the administrative support for such an internal plan.
As you can see from the above, when you ask us “Will this be covered?” we can’t really know. We are happy however to provide any insurance forms, resubmit forms if necessary, provide estimates, plus give suggestions and/or inform you of typical scenarios and rules.
As a final note, often you have to be the person to ask your insurance company the questions you want answered. Some companies are much stricter in their interpretation of how they comply with Privacy legislation and often will not talk to the dental office or answer questions from a dental office about a particular patient’s plan, saying it would be a violation of the privacy act and that the patient has to contact them personally. We do the best we can to help you deal with the dental insurance company, but there are limits to what we can do.
__________________________________________________
Dental Implants

Dental implants can be a great solution for people that are missing one or more teeth. Basically they are a titanium metal artificial root that is placed into the bone and allowed to heal. Then these artificial roots are used as anchors for the appliance that is used to replace the tooth or teeth. The implants are threaded inside so that the type of attachment needed can be screwed into the implant itself.
Several years ago it was discovered by accident that for items of pure titanium the bone does not just grow around it, it actually fuses to the metal. This means that retention of titanium implants of any type whether for hips, knees or teeth does not rely on some sort of screwed in physical retention but on the bone growing around the implant and fusing to the surface of the implant.
You hear people refer to screw in teeth but for dental implants where the screws actually come in are as a way to anchor things to the implant itself once it is fused to the bone. Examples of things that can be screwed into the implants are projections to cement an artificial tooth or bridge to, or anchors for metal bars for a denture to clip onto or individual anchors for a denture to snap onto.
Dental implants are not usually placed in a single one shot procedure. The usual way is for the implant to be surgically placed into a hole prepared in the bone and then left for a period of 3 – 6 months to allow the bone to heal around the implant and fuse to it. Once this has happened the dental implant is surgically exposed at the top and a “healing cap” is screwed into the implant. This is a short rounded extension that projects up through the gum and allows the gum to heal around it and produce a soft tissue cuff around the implant, similar to that around a natural tooth.
Once the gums have healed the healing caps are removed and whatever type of attachment being used is screwed into implant where the healing cap used to be. The attachments will now act as anchors to whatever type of artificial tooth or appliance is being placed.
While normally one of the best anchored and easiest to maintain tooth replacement options, there can be failures for a variety of reasons. Smoking for example can interfere with the process of bone fusing to the implant and many practitioners will not place implants on smokers for this reason.
Implants are usually the most expensive way of replacing missing teeth as well. Other forms of tooth replacement can be almost as expensive however and may not offer the advantages of dental implants.
Unfortunately most dental insurance plans do not cover the cost of dental implants but some of them will cover part of the cost of the crown or bridge (artificial teeth) that are anchored to the implants and at least reduce some of the cost to the patient.
__________________________________________________
Infection Control

The human mouth is not a sterile or clean environment. It is full of a wide range of bacteria and viruses even in clean healthy mouths. There is also the possibility of illness causing bacteria or viruses being present.
The purpose of infection control in a dental office is not to eliminate all of these bacteria and viruses in patient’s mouths but rather to prevent cross contamination between patients, and between patients and dental staff.
Infection control procedures are carried out making the basic assumption that you cannot know for sure what bacteria and viruses are present and whether they are capable of spreading disease so you assume all patients may have all possible disease causing organisms, even if it is unlikely, and protect against that scenario.
To do this a combination of various methods are used. Where possible and economically feasible disposable one time use items are used. Where these cannot be used, instruments are sterilized in sterilizers at high temperature. Larger things like chairs, lights and countertops that cannot be placed in a sterilizer are wiped down with disinfectants between patients.
The use of barriers is also another method. This includes wrapping some items in plastic for each use, or the use of gloves, masks and eye protection.
Basic hand washing or the use of hand sanitizers are also used to help prevent cross contamination.
With all this effort going into infection control patients sometimes wonder why they sometimes may still have an extraction site get infected. The reason is again that almost all of the precautions are to prevent cross contamination and you can still get an infection of an extraction site, etc., from the vast number of bacteria and viruses in your own mouth. With the number of micro-organisms in the mouth it should be more surprising that we don’t get far more infections but the majority of them are benign or even helpful and our immune systems are generally pretty effective.
__________________________________________________
Fluoride in Tap Water

Fluoride is often added to tap water as a public health measure to try and reduce the number of cavities in the population, especially in children. Some people express concern as fluoride in high concentrations can be toxic but in the levels used in tap water (one part per million) there have been no problems identified. Fluoride has been added to many water supplies at this level for many years and no negative results have been noted.
Most people see fluoride in water as a totally artificial man made phenomenon but this is not true. Many natural water supplies have fluoride in them. In fact this is how the dental benefits of fluoride were first discovered. A dentist was practicing in two separate small towns and noticed that there was a marked difference in the number of cavities between the two towns. The cause for the difference in the number of cavities was traced to the fluoride levels in the two town water supplies. The town with far fewer cavities had natural high levels that had not been added by humans but rather came from the rocks of the water source.
It is possible for natural sources of fluoride in water to be at toxic levels but when it is added to municipal water supplies the levels are carefully regulated and controlled.
The use of fluoridation to help control cavities is recommended by dental organizations and the World Health Organization.
__________________________________________________
TMJ Disorders

The temporomandibular joint (TMJ) acts like a sliding hinge, connecting your lower jaw to your skull. This is one of the most complex joints in the body.
TMJ disorders can cause pain in your jaw joint and in the muscles that control jaw movement. The pain can also feel like a headache on the side of the head or an ear ache as well.
The exact cause of a person’s TMJ disorder is often difficult to determine. Your pain may be due to a combination of problems, such as arthritis or jaw injury. Some people who have jaw pain also tend to clench or grind their teeth, but many people habitually clench their teeth and never develop TMJ disorders. There seems to be a threshold below which no symptoms are noted and above which TMJ pain results.
In most cases, the pain and discomfort associated with TMJ disorders can be alleviated with self-managed care or nonsurgical treatments. Severe TMJ disorders may require surgical repair
Signs and symptoms of TMJ disorders may include:
- Pain or tenderness of your jaw
- Aching pain in and around your ear
- Difficulty chewing or discomfort while chewing
- Aching facial pain
- Locking of the joint, making it difficult to open or close your mouthConsult your dentist if you have persistent pain or tenderness in your jaw, or if you can’t open or close your jaw completely. Your dentist can discuss possible causes and treatments of your problem. Painful TMJ disorders can occur if:
- The temporomandibular joint (TMJ) combines a hinge action with sliding motions. The parts of the bones that interact in the joint are covered with cartilage and are separated by a small shock-absorbing disk, which normally keeps the movement smooth.
- TMJ disorders can also cause a clicking sound or grating sensation when you open your mouth or chew. But if there’s no pain or limitation of movement associated with your jaw clicking, you may not need treatment for a TMJ disorder.
- The disk erodes or moves out of its proper alignment
- The joint’s cartilage is damaged by arthritis
- The joint is damaged by a blow or other impact
Treatment can range and may include medications, exercises, an appliance to help control clenching or grinding habits, or in severe cases that don’t resolve with less invasive methods, surgery. Usually treatment starts with less invasive methods and only progress further if those prove unsuccessful.
TMJ disorders most commonly occur in women between the ages of 20 and 40, but may occur at any age and in men as well.
__________________________________________________
The Power of a Smile
The power of a smile is so great that it even acts across species barriers. The big smile of the chimpanzee above makes you want to smile or laugh yourself. Admit it.
It is something we often do automatically and without thought. If there is something we find funny or if we feel happy, we smile.
The physical action of smiling triggers activity in the parts of the brain that register happiness. Happiness makes you smile and smiling helps make you feel happy. It works in both directions.
Smiling can make you happy, it can help you reduce feelings of stress, it helps others feel happier and studies have shown it makes you look more attractive to others. Last but not least, smiling can lead to laughter which is even better for you.
Don’t let being self-conscious about your smile make you lose out on all these benefits. If you would like to feel better about your smile and feel more comfortable about smiling a lot more, check with your dentist about options to improve your smile. There are many options available to improve your smile so you can feel like smiling with everyone else.
__________________________________________________
